The Problem
Separate vertical programs and related disconnects result in inefficient functioning of health systems
of low- and middle-income countries. Furthermore, weaknesses in primary health care
including inadequate staff force, challenges in implementation of monitoring and governance frameworks, inefficient paper-based systems leading to transparency challenges, and underperformance of primary health care providers within the community further compound the situation, resulting in poor health outcomes. Pakistan is one of the two countries in the world where polio remains endemic, and there is a need for provincial health systems to implement innovative, effective, and efficient solutions for Pakistan to achieve the Sustainable Development Goal targets of Maternal Mortality Ratio of 70 and the under-five mortality of 25 by 2030.
The Solution
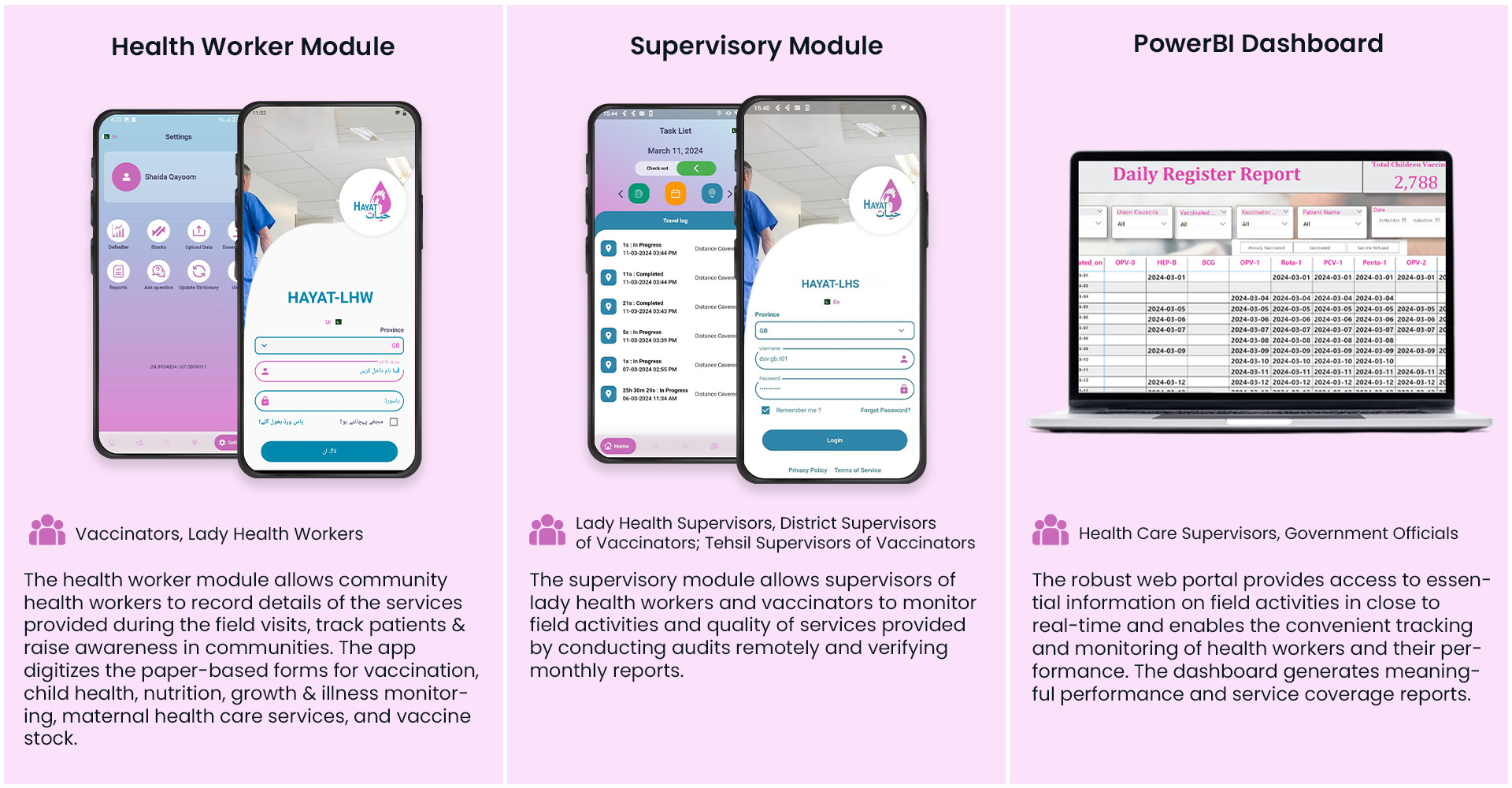
Hayat is a novel mHealth application, which aims to empower health workers with technologies to improve coverage of and access to Reproductive, Maternal, Newborn and Child Health (RMNCH), immunization and child growth services. Hayat achieves this by streamlining healthcare worker operations through digitalization. The program prioritizes the well-being of children under two years old and women of reproductive age residing in targeted catchment areas within Gilgit-Baltistan (GB) and Chitral, Khyber Pakhtunkhwa (KPK).
Pilot and scale-up evaluations demonstrated significant improvements in health worker attendance, service satisfaction, and key maternal and child health outcomes including improved vaccination rates and skilled birth attendance.
Evaluation Findings
Hayat is currently undergoing its final transition-to-scale phase (TTS4). This evidence-based intervention has been rigorously evaluated throughout its implementation. TTS4 included cross-sectional surveys with key stakeholders across the Pakistani health system, encompassing decision-makers, provincial and district leadership, and both administrative and field personnel. The surveys assessed the potential for integration and long-term sustainability of Hayat. This evaluation focused on three core categories: core system readiness, technological infrastructure readiness, and societal acceptance.
The findings reveal a strong understanding among health professionals of Hayat's potential to address critical needs. Additionally, there is a demonstrable commitment from the government to expand digital technology infrastructure in previously underserved regions. However, policymakers and politicians exhibit a gap in awareness regarding digital health solutions like Hayat. Pakistan's political landscape presents challenges, as past policies promoting technology adoption have seen limited execution. Additionally, while telemedicine is gaining popularity in support of its dissemination, there are still limited published standards for mHealth tools like Hayat.
Qualitative Findings
Qualitative research conducted in 2020 (Zaidi et al., 2020) assessed the intervention's usability, operability, and task-technology fit to inform its long-term sustainability within the health system. Findings indicated positive user acceptance among Pakistani healthcare providers, who appreciated the convenience of using the Hayat app on their smartphones. The app demonstrably contributed to a more reliable and transparent health system by facilitating improved data tracking for frontline workers and clients. Notably, the research revealed user-friendliness for both end-users and stakeholders at the district level. Platform adoption has yielded demonstrably improved data quality and timeliness, leading to enhanced immunization coverage and maternal care through more effective supervision and monitoring of community health workers and lady health workers. The enhanced validity and reliability of data collected through the app has instilled greater confidence in health managers' decision-making processes.
Scaling and Sustainability through Government Partnerships
The Hayat platform has received strong support and demand from the health systems in GB and KPK, despite administrative and political challenges. The project has established partnerships at multiple tiers of the health system, and the platform has been upgraded for expansion into remote regions.
Due to the project’s successful implementation, encouraging results in improving health outcomes, and positive uptake by multiple tiers of the health system, the project currently being scaled in additional districts of Gilgit-Baltistan, including Astore, Diamer, Hunza, Skardu and Nagar. Similarly. the Department of Health, KPK is now considering Hayat for implementation across the province of KPK.
Hayat has been implemented by the Aga Khan University in collaboration with Aga Khan Health Service, Pakistan and local government partners. It is funded by the Government of Canada, through the Grand Challenges Canada and the Aga Khan Foundation Canada.